Eligibility Verification
Providers are responsible for verifying eligibility every time a member is seen in the office. PCPs should also verify that a member is assigned to them.
Medicaid eligibility in Florida is determined either by the Department of Children and Families (DCF) or the Social Security Administration (SSA), which determines eligibility for individuals receiving Supplemental Security Income (SSI). DCF determines Medicaid eligibility for:
- Parents and caretaker relatives of children
- Children
- Pregnant women
- Former foster care individuals
- Non-citizens with medical emergencies
- Aged or disabled individuals not currently receiving Supplemental Security Income
- (SSI)
Medicaid and Medicaid Specialty Plans
Until the actual date of enrollment with the plan, Sunshine Health is not financially responsible for services the prospective member receives. In addition, Sunshine Health is not financially responsible for services members receive after coverage is terminated. However, Sunshine Health is responsible for anyone who is a Sunshine Health member at the time of a hospital inpatient admission and changes health plans during that confinement.
Comprehensive Long Term Care
Sunshine Health is responsible for providing LTC services once the Florida Department of Elderly Affairs determines an enrollee meets the medical requirements for nursing home level of care and the enrollee formally selects the Sunshine Health Comprehensive plan through AHCA’s Choice Counseling. Following that selection, the Department of Children and Family Services (DCF) determines if the member meets the financial criteria. Once AHCA receives confirmation of a member’s eligibility, AHCA notifies Sunshine Health of the member’s effective enrollment date. Coverage typically lasts for a year until DCF recertifies the member. During the annual recertification process, Comprehensive members may receive a 60-day extension of coverage and their benefit category is changed to “SIXT” on the secure provider portal of AHCA’s website.
Verifying Member Eligibility
Sunshine Health recommends providers verify eligibility before rendering services for our members and at least monthly for Comprehensive members. Providers may use the Secure Provider Portal to verify member eligibility or use the tools and resources provided by AHCA for that purpose.
Providers must verify a member’s eligibility each time a member schedules an appointment and arrives for services. Because members may change PCPs and health plans, PCPs should also verify that a member is their assigned member. Sunshine Health must authorize all services before providers render any LTC-covered service for Comprehensive members.
Methods to Verify Eligibility
- Providers are asked to verify member eligibility by using the Sunshine Health secure provider portal. Using the portal, any registered provider is able to quickly check member eligibility by indicating the date of service, member name, and date of birth or the Medicaid ID number and date of birth.
- Providers may call Provider Services at 1-844-477-8313. Providers are asked to supply the member’s name and date of birth or the member’s Medicaid identification number and date of birth.
- You may also verify benefits through the Florida Medicaid Secure Web Portal (FLMMIS)
- Availity Essentials: Log into your account
ID Cards
Medicaid
MMA, Comprehensive Long Term Care, Sunshine Health Sunshine Health Mindful Pathways Specialty Plan (SMI), Sunshine Health Power to Thrive Specialty Plan (HIV)

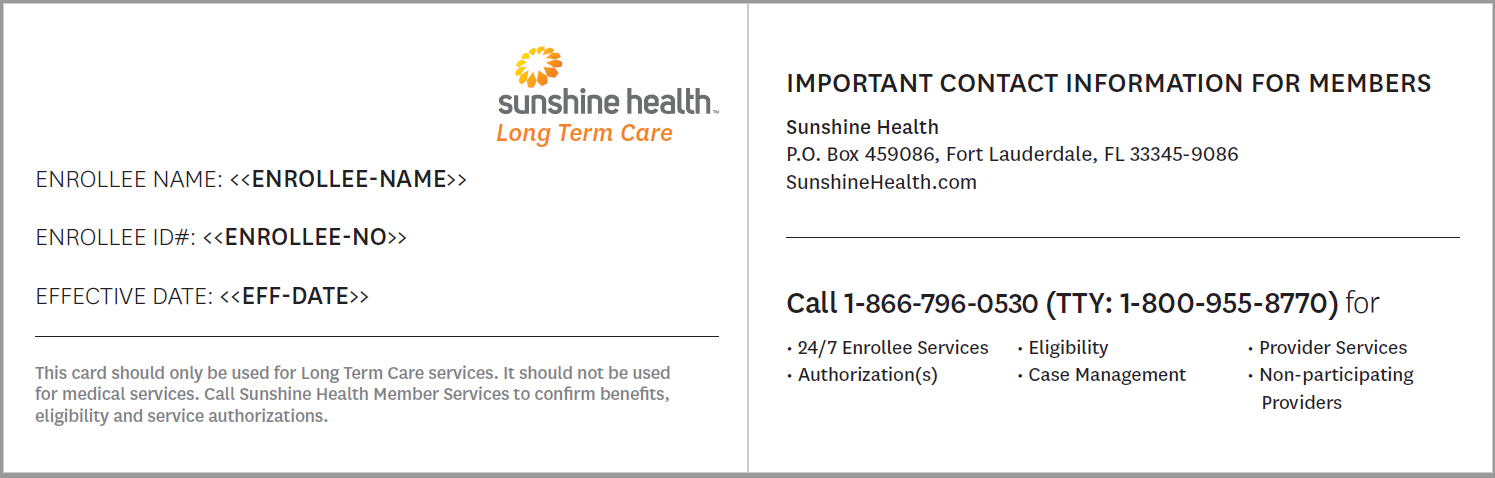
Long Term Care
Sunshine Health Pathway to Shine Specialty Plan (CW)

