Behavior Analysis (BA) — Provider Quick Reference Guide
Important Contact Information
- Provider Services
- All products
- 1-844-477-8313
- Monday-Friday from 8 a.m. to 8 p.m. Eastern
- Pharmacy Services
- All products
- 1-800-460-8988, option 2
- 24 hours a day, 7 days a week
- Member Services
- Comprehensive MMA, SMI, HIV/AIDS
- 1-866-796-0530
- Monday-Friday from 8 a.m. to 8 p.m. Eastern
- Sunshine Health Pathway to Shine Child Welfare Specialty Plan (CWSP)
- 1-855-463-4100
- Monday-Friday from 8 a.m. to 8 p.m. Eastern
- Children's Medical Services (CMS) Health Plan Title 19 and Title 21
- 1-866-799-5321
- Monday-Friday from 8 a.m. to 8 p.m. Eastern
- Ambetter
- 1-877-687-1169 (Relay Florida 1-800-955-8770)
- Monday-Friday from 8 a.m. to 8 p.m. Eastern
- Comprehensive MMA, SMI, HIV/AIDS
Verifying Member Eligibility
These suggestions are not a guarantee of coverage.
- Verify member eligibility by using the Sunshine Health Secure Provider Portal to confirm eligibility quickly and efficiently.
- Using the portal, any registered provider is able to quickly check member eligibility by entering the member’s name and date of birth, or Medicaid ID number and date of birth, along with the date of service.
- It is essential to select the correct “Plan Type” when performing an eligibility search to ensure accurate results.
- Member Coordination of Benefits (COB) information can also be found in the Secure Provider Portal.
- Alternatively, you can call Provider Services at 1-844-477-8313. Please provide the member's name and date of birth or their Medicaid ID number and date of birth.
Member ID Cards
Sunshine Health (Comprehensive MMA, CWSP, SMI, HIV/AIDS)
Children Medical Services (CMS) Title XXI (21)
Children Medical Services (CMS) Title XIX (19)
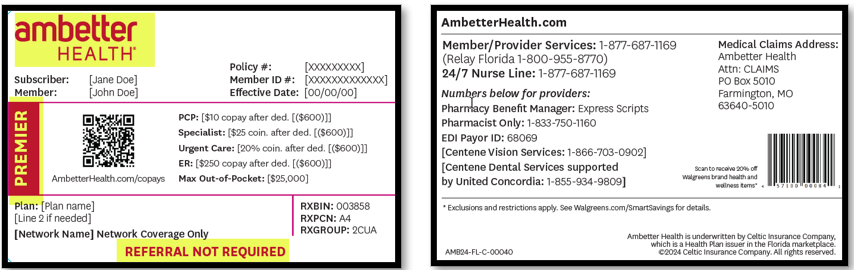
Ambetter Premier (formerly known as Core)
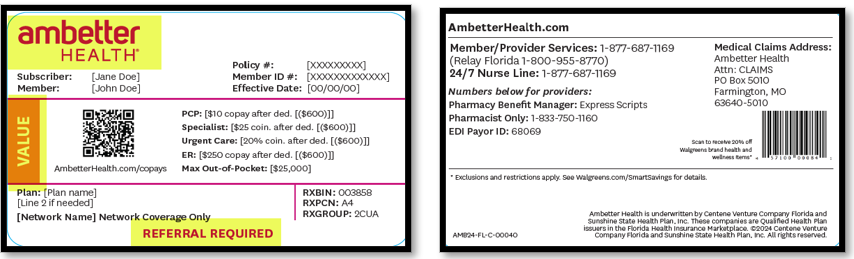
Ambetter Value
Definitions:
- MMA (Managed Medical Assistance): This Medicaid program provides comprehensive medical and behavioral health services, including ABA services, to Medicaid recipients who opted out of a specialized plan.
- SMI (Sunshine Health Mindful Pathways Specialty Plan): This Medicaid program offers medical and behavioral health services, including ABA services, to members aged 6 and older who have one or more of the following conditions: psychotic disorders, delusional disorder, bipolar disorder, schizoaffective disorder, obsessive-compulsive disorder and major depression.
- CWSP (Sunshine Health Pathway to Shine Specialty Plan): This Medicaid program provides medical and behavioral health services, including ABA services, to children in the child welfare system, including those in foster care, receiving adoption services, or at risk of being removed from their homes.
- HIV/AIDS (Sunshine Health Power to Thrive Specialty Plan): This Medicaid program offers specialized healthcare services to individuals living with HIV/AIDS.
- Children Medical Services (CMS): This program is designed for individuals who are eligible for Medicaid or KidCare and have special healthcare needs.
- CMS Title XIX (19): This Medicaid program provides medical and behavioral health services, including ABA services, to members ages 0-20 years with special healthcare needs who qualify for Medicaid coverage. There is no copayment or premium cost to the member.
- CMS Title XXI (21): Children’s Health Insurance Program (CHIP): This program provides medical and behavioral health services, including ABA services, to children ages 0-18 years with special healthcare needs who qualify for KidCare. These individuals are not Medicaid recipients. There may be a copayment or premium cost for the member, which is determined by family income.
- Ambetter Health/Marketplace
- Premier Plan: This product has our broadest network of healthcare providers and hospitals.
- Value Plan: This product has select healthcare providers and hospitals in the network. This plan requires a referral to providers outside the members’ assigned Primary Care Provider.
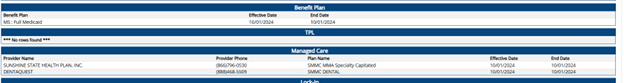
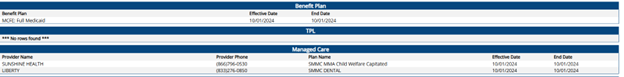
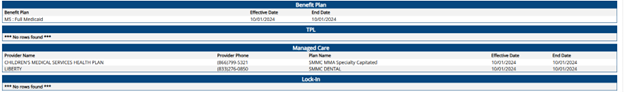
Breakdown of Applicable Products in FLMMIS
Please review below examples of how each plan product will appear in Florida Medicaid Management Information System (FLMMIS).
Product Name | FLMMIS Provider Name | FLMMIS Plan Name |
|---|---|---|
Managed Medical Assistance (MMA) | Sunshine Health | SMMC MMA Capitated |
Sunshine Health Pathway to Shine (CW) | Sunshine Health | SMMC MMA Child Welfare Capitated |
Sunshine Health Mindful Pathways (SMI) | Sunshine Health | SMMC MMA Specialty Capitated |
Children’s Medical Services (CMS) Title 19 | Children’s Medical Services Health Plan | SMMC MMA Specialty Capitated |
Children’s Medical Services (CMS) Title 21 | N/A | N/A |
Managed Medical Assistance (MMA)
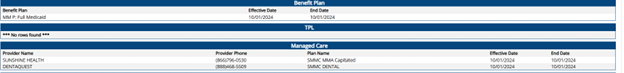
Sunshine Health Mindful Pathways (SMI)
Sunshine Health Pathway to Shine (CW)
Children’s Medical Services (CMS) Title 19
BA Authorizations
Prior authorization is required for all BA services.
Prior-authorization requests are processed by Sunshine Health’s Utilization Management (UM) Department.
- MMA, CW, SMI, LTC, HIV: Determination within 5 calendar days of receipt of request.
- CMS: Determination within 7 calendar days of receipt of request.
- BA prior authorization requests can be submitted for up to 6 months of services.
Submit authorization requests via one of the following:
- Online: via the Sunshine Health Secure Provider Portal
- Utilization Management Phone number: 1-844-477-8313
- BA Fax: 1-844-208-9113
- Standard hours of operation: Monday- Friday from 8 a.m. to 8 p.m. Eastern
- Weekend and After-Hours on Call-Numbers (For All Products): 1-844-477-8313
Required Documentation
All documentation must reflect the individual assessments, needs and interventions of the recipient.
Initial Behavior Assessment and Behavior plan requests:
- A referral for BA services is required as follows:
- The recipient must be referred by an independent physician or practitioner qualified to assess and diagnose disorders related to functional impairment, including:
- Primary care physician with family practice, internal medicine or pediatrics specialty;
- Board certified or board eligible physician with specialty in developmental behavioral pediatrics, neurodevelopmental pediatrics, pediatric neurology, adult or child psychiatry
- Child psychologist
- The recipient must be referred by an independent physician or practitioner qualified to assess and diagnose disorders related to functional impairment, including:
Comprehensive Diagnostic Evaluation (CDE)
A comprehensive diagnostic evaluation (CDE) performed according to national evidence-based practice standards. CDEs may be performed by a multidisciplinary team or individual practitioner. In any case, the CDE must be led by a licensed practitioner working within their medical, developmental, or psychological scope(s) of practice. The CDE must include assessment findings and treatment recommendations appropriate to the recipient. For example, the CDE may include data from behavioral reports by parents, guardians, and/or teachers; diagnostic testing related to recipients‘ development, behavior, hearing, and/or vision; genetic testing; and/or other neurological and/or medical testing.
Behavior Assessment and Behavior Treatment plan
- Providers should request re-assessment units with their treatment request.
- Florida Medicaid Behavior Analysis service policy identifies a 40-hour per week limit for behavior analysis services.
- Behavior assessment and behavior plan with specific criteria are listed in the Florida Medicaid Behavioral Analysis Coverage Policy (PDF).
- The behavior assessment and behavior plan must be signed by the Lead Analyst and the recipient’s parent or guardian.
- The Vineland-3 and BASC-3 PRQ core assessments are required to be included for initial assessment and annually for reassessments.
- The complete scoring reports for the Vineland and BASC, including outcome measure scores, must be submitted with service at each prior authorization request.
Assessment and Behavior Plan for Reauthorization and Continuation of Services
- In addition to the documentation requirements indicated in Florida Medicaid Behavioral Analysis Coverage Policy (PDF), assessments and behavior plans for reauthorization and continuation of services must include:
- Data reflecting progress of all behaviors targeted for improvement. Each behavior under treatment must have its own data table and corresponding graph. A narrative discussion of progress and a statement of justification for continuation of care at the intensity level requested. If significant clinical progress is not made over the course of an authorization period, the provider must explain why clinically significant progress was not made and treatment changes to promote progress.
Note: Please use the Treatment/Service Request Forms for fax submission.
BA services must be rendered by one of the following:
- Lead Analysts who are one of the following:
- Board certified behavior analyst (BCBA) credentialed by the Behavior Analyst Certification Board.
- Florida certified behavior analyst (FL-CBA) credentialed by the Behavior Analyst Certification Board.
- Practitioner fully licensed in accordance with Chapters 490 or 491, F.S., performing within their scope of practice.
- Board certified assistant behavior analysts (BCaBA) credentialed by the Behavior Analyst Certification Board working under the supervision of a BCBA.
- Registered behavior technicians (RBT) credentialed by the Behavior Analyst Certification Board working under the supervision of a BCBA or BCaBA.
Utilization Management Decisions
- Decision letters will indicate options for providers to either file peer-to-peer (P2P) or a medical appeal. The decision letter will include instructions for those options.
- For peer-to-peer requests, use our peer-to-peer form within two business days of the decision letter.
- You can also call 1-844-477-8313, ext. 6032912 within two business days of the decision letter.
- For more details about the medical appeal process, visit the Medicaid Appeals Guide (PDF).
- Member Appeal: May be filed by the member or the member’s representative, including providers with the member’s signed consent. This must be filed within 60 days from the date of the Notice of Adverse Benefit Determination (NABD) or
- Provider Appeal: May be filed by the direct service provider or the member’s PCP.
- First-Level Appeal (Reconsideration): Must be filed within 90 days from the original explanation of the decision letter or Explanation of Payment (EOP).
- Second-Level Appeal (Dispute): Must be filed within 90 days from the original Appeal Denial Notice.
Claims
Behavioral Analysis (BA) Covered Services
Behavior analysis (BA) services are covered for all Sunshine Health Medicaid and CMS Health Plan Title 19 and Title 21 members. For more information about covered services, refer to AHCA’s Behavior Analysis Services Provider Information resource.
Methods for Claims Submission
For both paper and electronic data interchange (EDI) claim submissions, the appropriate Center for Medicare and Medicaid Services (CMS) billing forms are required:
- CMS 1450 (UB04) for facilities.
- CMS 1500 for professionals.
- There are several ways to submit claims to us:
- Paper Claims: The Sunshine Health Provider Manual has detailed instructions.
- Electronic Data Interchange (EDI): Consult the Sunshine Health Provider Manual.
- Secure Provider Portal: Visit the Secure Provider Portal.
- Availity Essentials (Preferred method for non-participating providers): Log into your account or register now. For assistance, please call Availity Client Services at 1-800-AVAILITY (1-800-282-4548). The Availity platform also has virtual training available.
Secure Provider Portal
- Participating (PAR) and Non-Participating (Non-PAR) providers interested in billing directly to Sunshine Health's provider portal can do so via the Secure Provider Portal.
- PAR and Non-PAR providers can gain access to Sunshine Health's portal by following these steps:
- Providers must add their Taxpayer Identification Number (TIN) to Sunshine's back-end system.
- PAR: Provider must complete the JON (Join Our Network) process (Contracting, Credentialing, etc.).
- Non-PAR: Provider must file a clean claim to Sunshine Health.
- Once a TIN is loaded in our system, please wait at least two business days to be added to our system (this applies to PAR and Non-PAR providers.)
- To determine if a claim has made it through our front-line claims edits, please contact:
- Sunshine Health Provider Services: 1-844-477-8313
- Ambetter Health Provider Services: 1-877-687-1169
- Providers must add their Taxpayer Identification Number (TIN) to Sunshine's back-end system.
Claims Submissions
Health Plan | Claim Type | Payer ID # | Paper Claim Mailing Address |
|---|---|---|---|
Sunshine Health, CMS, SMI, CWSP, HIV/AIDS | Professional and Institutional | Sunshine Health: 68069
| Attn: Claims Department P.O. Box 3070 Farmington, MO 63640- 3823 |
Ambetter Health | Professional and Institutional | 68069 | Attn: Claims Department P.O. Box 5010 Farmington, MO 63640-5010 |
Billing
In general, Sunshine Health follows Centers for Medicare & Medicaid Services (CMS) billing requirements. Please refer to your contract to determine contracted products, negotiated rates and Fee Schedules. For additional questions, contact Sunshine Health Provider Services at 1-844-477-8313.
- We process payment cycles four times per week to ensure payments are consistently being issued.
- Providers should allow 5-7 business days for clean claims to process.
- New providers who have never billed us should allow a few additional days.
- Adjusted claims, requests for reconsideration and disputed claims will be finalized to a paid or denied status 30 calendar days of receipt.
For additional questions, contact Sunshine Health Provider Services at 1-844-477-8313 or Ambetter Health Provider Services at 1-877-687-1169.
Important Links
- Provider Reimbursement Schedules and Billing Codes
- Behavioral Analysis Services Information
- Sunshine Health Provider Manuals, Forms and Resources
- Sunshine Health Billing and Claims
- Ambetter Health Provider Resources
- Behavior Analyst Certification Board
- Agency July 29, 2022, BA Fee Schedule Training: Fee Schedule Webinar Recording
Timely Claim Submission
Providers must submit claims in a timely manner as indicated in the following table.
Initial Claim* | Reconsiderations or Claim Dispute** | Coordination of Benefits*** | |||
|---|---|---|---|---|---|
Participating | Non-Participating | Participating | Non-Participating | Participating | Non-Participating |
180 days | 365 days | 90 days | 180 days | 90 days | 90 days |
*In an initial claim, days are calculated from the date of service to the date received by Sunshine Health.
** In a reconsideration or claim dispute, days are calculated from the date of the explanation of payment/correspondence issued by Sunshine Health to the date the reconsideration is received by Sunshine Health.
*** For coordination of benefits, days are calculated from the date of explanation of payment from the primary payer to the date received by Sunshine Health.
Overpayment Refund Address
When a facility, group or practice identifies an overpayment, a refund should be submitted to the address indicated below and include all applicable claims for which the refund is being submitted.
Sunshine Health
Attn: Centene Mgmt. Co - Sunshine State Health Plan
P.O. Box 947986
Atlanta, GA 30394-7986
Remittances and Payspan
If you are currently receiving paper checks and would like to switch to Electronic Funds Transfer (EFT), please register with Payspan.
Register by visiting Payspan’s website, calling 1-877-331-7154 or emailing providersupport@payspanhealth.com. If your address is incorrect in Payspan, please update it.
Update Provider Demographics
Providers can use the Provider Demographic Updates form to quickly update their practice information like their phone number, hours of operation, or address.
Credentialing and Provider Changes
To add a new practitioner or facility to your existing Sunshine Health contract, please visit the Practitioner Enrollment Request page. This form is restricted for adding a practitioner or facility to an existing, contracted group. If the tax ID is not currently contracted with Sunshine Health, please submit a request to Join Our Network. If a request is submitted for a non-contracted group, the request will be returned to you unprocessed.
To become a participating Registered Behavioral Technician (RBT) with Sunshine Health, you must be board certified by the Behavior Analyst Certification Board when you submit your request to participate in our network. During our enrollment process, if BACB certification cannot be verified, we cannot process the request. You do not need to submit a screenshot or proof. Sunshine Health will verify through the BACB.
For RBTs contracted with Medicaid products, a valid, active and enrolled Medicaid ID must be validated against AHCA’s Provider Master List. This requirement does not apply to Marketplace or Medicare products.
Important: Practitioners should not begin servicing Sunshine Health members until they have received a Provider Enrollment Confirmation letter from Sunshine Health’s Provider Enrollment department. Our enrollment process can take up to sixty (60) days to complete. We will not backdate effective dates due to services provided ahead of the practitioner’s enrollment. For more information, visit:
BCBA/BCaBC Credentialing Requirements
- LOAP (XLSM)
- CAQH or Sunshine Health Application: Must be attested within 120 days (CAQH page 5 specialty must match the specialty requested)
- Malpractice insurance or financial responsibility: Minimum amount of $250,000 to $750,000
- Work history: The last five years and must include the current group being linked to
- Specialty profile form
- Active Medicaid number with taxonomy matching specialty requested (For Medicaid LOB only)
- Must have an active certification (BACB certification verification)
Contracting
Sunshine Health takes proactive actions that are aimed at creating a comprehensive and high-quality network that meets the needs of its members while ensuring access to necessary services. If you are a non-contracted provider, please submit your request to join our network.
Note: Submitting this inquiry is an important first step in the process, but it does not guarantee entry into our network. This form is different from a credentialing application or a signed agreement. The information you provide will be used solely by Sunshine Health to evaluate the potential for offering a new contract, amending an existing one, or adding an additional product to an existing contract. We appreciate your interest and will carefully review your submission.
All contract rate discussions for participating providers are unique and confidential, if you have questions please email sunshinecontracting@sunshinehealth.com and a representative will reach out to speak with you.
24-Hour Nurse Advice Line and Crisis Line
The Nurse Advice Line can assist providers with checking member eligibility. It can also connect members to telemedicine for urgent care visits. The same number also has a Behavioral Health Crisis Line. Hours of operation are 24 hours a day, 7 days a week.
- CMS: 1-866-799-5321 and follow prompts for Nurse Advice Line, Option 1, then select Option 7.
- MMA and SMI: 1-866-796-0530 and follow prompts for Nurse Advice Line, select Option 1, then Option 3, then Option 5.
- CWSP: 1-855-463-4100 and follow prompts for Nurse Advice Line, select Option 1, then Option 2, then Option 5.
- Ambetter Health: 1-877-687-1169 (Relay Florida 1-800-955-8770). Available 24-7, 365 days a year.
988 — Suicide & Crisis Hotline
If you are struggling with alcohol or drug use, experiencing ongoing anxiety or depression, or experiencing a crisis, dial or text 988, or chat with a trained counselor at 988lifeline.org/chat. This service is confidential, free of charge, and available 24/7, 365 days a year.
Provider Engagement
Sunshine Health has a team of Provider Engagement Account Managers throughout Florida, who are committed to supporting providers and addressing your needs. Learn more about how Provider Engagement can help you.
Our Account Managers are available to assist with a variety of services designed to support the success of your practice. These professionals spend three or more days each week directly engaging with providers in the field.
For inquiries related to operational issues, we kindly ask that you direct these to our dedicated providers service team at 1-844-877-8313 who are equipped to handle those requests promptly and efficiently.
To identify your designated Account Manager, visit our Find Your Account Manager tool.
Additional Resources
- Access and Availability Timeframe Standards: Sunshine Health establishes and assesses compliance with appointment wait times for various types of visits. Please view Standards for Appointment Scheduling.
- Find A Provider (FAP) Tool: If you need assistance locating a specialist or facility for a member, please visit our Find a Provider tool. Here you will be able to search by provider name, NPI and specialty type.
- Community Resources: Our Sunshine Health Community Resource Database connects members and caregivers in need with local programs and supports.
- For Providers: Stay up to date on provider communication by visiting For Providers and Provider News. On this page, providers can also subscribe to our monthly newsletter.
- Vendors: Contact information for Sunshine Health’s subcontractors and vendors.
FAQ: Behavior Analysis (BA) Frequently Asked Questions
Updated: December 2, 2025
Claims & Billing
- What steps should be taken when a provider receives an error code during web portal claim submission?
- No action is required until the claim shows finalized (paid/denied).
- When a member has other primary insurance, what are the best practices for submitting to the health plan?
- Medicaid will always be secondary when the member has another carrier. If the primary carrier denies the services, the explanation of payment (EOP) must be submitted to the health plan with the claim. We will need to EOP to coordinate the member’s benefits.
- How do we handle claims that have a Third-Party Liability?
- Claims for which there is another insurance carrier should be billed to the primary payor and submitted with primary EOB for payment.
- The member’s coordination of benefits (COB) was updated to show the member did not have primary coverage at the time services were rendered. What is my next step?
- Please send the Claims Template (XLSX). We will check the member’s third-party liability, and if/once it is updated, the claims can be reprocessed.
- How do we proceed with billing the codes with XP Modifiers? With Medicaid they request for us to bill at least $0.01 for the system to accept the claim. How many units should be billed? Will this reduce the available auth units?
- To ensure Medicaid claim acceptance for codes 97153XP and 97155XP, continue to bill with a minimum charge of $0.01. This minimal billing prevents claim denials while maintaining compliance with Medicaid. Consistently use the XP modifier for these codes and ensure all documentation supports the service provided.
- Should we bill both RBT on one claim (EQ Health allowed them to be billed for them together in one claim form)?
- Sunshine Health requires separate claim submissions for RBT services rather than combined claims.
- What protocol should we follow when submitting claims if the recipient received services in the morning at school with one Registered Behavior Technician (RBT) and then additional services in the afternoon with another RBT? If the claim denies for duplicate in error, should we file a reconsideration or just wait for the system to update and fix itself ?
- Sunshine Health is reimbursing providers for these services, therefore, please do not hold your claims. You can bill Sunshine Health immediately.
- What is the process to submit claims for the same rendering provider to avoid duplicate denials (denial code EX18)?
- To prevent duplicate denials, providers should submit a single claim when billing for the same rendering provider on both the morning and afternoon of the same day.
- What do I need to do if I receive a EX18 denial?
- If an RBT is billing for the same member, on the same date, with the same procedure code, multiple times per day, then those services should be submitted on a single claim form to avoid duplicate denials.
- To ensure proper processing and payment, please resubmit via one single corrected claim.
Direct Deposit
- Do we have to have a paid paper claim to have access to Payspan? Or can the claim be submitted electronically?
- Payspan has to be able to validate the Tax ID number with us. If you are already loaded in the system, you should be able to call Payspan to register.
- If you are not loaded with us, a claim has to be billed, but it does not have to be a paper claim. It can be submitted electronically. The first claim submission will come back in form of paper EOP and will indicate a registration code.
- Payspan has to be able to validate the Tax ID number with us. If you are already loaded in the system, you should be able to call Payspan to register.
- My group is already set up for EFT through Payspan. We continue to add several billing NPIs to our agreement. What is recommended as the best next, step in this scenario?
- We recommend providers contact Payspan to ensure your organization is set up properly.
Provider Training
- When are the next ABA Provider Town Hall sessions?
- Behavior Analysis (BA): Wednesday, April 22, 2026
- Behavior Analysis (BA): Wednesday, February 4, 2026
- Visit Provider Training to register for training sessions and view recordings of past sessions.
Provider Updates
- Where should provider updates for RBT to BCBA transitions be submitted?
- This change should be submitted as a "Specialty change" using the Provider Demographics Update (PDU) tool. However, the specialty must be updated with AHCA first and reflected on the Provider Master List (PML). Upon receipt of the request through the PDU tool, please allow up to 30 days to process the request. You will receive a confirmation notice once the change has been processed.
Credentialing
- Is it okay to list the RBT Requirements Coordinator as the supervising analyst because some RBTs may have more than one analyst as a supervisor across members?
- RBTs assist in delivering behavior-analytic services and practice under the direction and close supervision of an RBT Supervisor and/or an RBT Requirements Coordinator, who are responsible for all work performed by RBTs. Sunshine Health will accept the RBT Requirements Coordinator as a supervising clinician.
Authorizations
- Are authorizations submissions an available function through Availity?
- Authorizations can be submitted through both the Availity Login and the Sunshine Health Secure Provider Portal, giving providers multiple options for submitting authorization requests. Either platform can be used to complete and process authorization submissions.
- What is the procedure for submitting a modification request after an authorization has been approved?
- This process has not changed. Please reach out to our Utilization Management team and request the updates. We prefer fax for these changes.
- What do members who are changing from one insurance to another need to do?
- Providers do not need to do anything or send anything additional to make us aware.
- Please note, claims should be directed to Sunshine Health for further processing.
- What do I need to do if member is changing from one provider to another?
- If services are moving from one agency to another agency, a new prior authorization is required. Use the member Change of Provider form (PDF).
Network and Contracting
- How will provider credentialing align with the new contract start date?
- Provider credentialing documentation will be collected concurrent with contract creation. Upon contract execution, all documentation will be processed to ensure provider credentialing is completed prior to the contract effective date.
- Any members they bill for now will be paid even if they have not been credentialed due to the COC.
- How long does the contracting process take?
- Once the contract is signed and submitted, it can take up to 60 days to process and load into our systems. You should continue to submit claims during the processing period.
Sunshine Health Secure Provider Portal
- I am a non-participating provider and I need access to the portal. How is this done?
- You must submit a claim to Sunshine Health and allow it to process. The Taxpayer Identification Number (TIN) in the system is how it will reflect in the Secure Provider Portal.
Availity Essentials Portal & Member ID Cards
- Does Availity cost money to use?
- No, Availity is free for providers.
Member Information
- Do members have a choice in health plan coverage?
- Members have the choice through the open enrollment period to pick a health plan.
- Under the SMMC program, there are different methods for enrolling, disenrolling and changing from one health plan to another. For more information, visit the AHCA Enrolling in a Health Plan guide.
Telehealth
- What are the telehealth requirements from a BCBA providing caregiver training to a client with Sunshine Health or CMS insurance? Must they reside within the state? Should they use a specific HIPPA compliant platform?
- We follow the guidelines outlined by AHCA in the Florida Medicaid Behavior Analysis Services Coverage Policy and the Florida Statues.
- Out-of-state providers must be registered with the Florida Department of Health.
- The telehealth platform must be compliant with HIPAA.